-
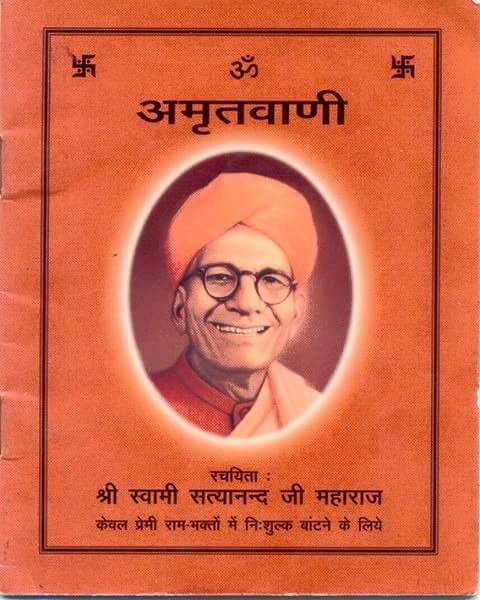 Amritwani
Amritwani
-
 Bhajans
Bhajans
-
 Ramayan
Ramayan
-
 Bhakti Prakash
Bhakti Prakash
- Dhun
- Search
- New Clips
- Top Hits
- Catogeries
- Artists
Browse Clips
© 2026 Ramsharnam Bikaner
No tracks found
Info
- 0 Tracks
- Male
- Social Links
- Bio
-
First Steroid Cycle: Best Steroids For Beginners
# A Comprehensive Guide to Popular Body‑Building Drugs
*(For informational purposes only – do not use without medical supervision)*
---
## 1. Why Athletes Turn to Anabolic‑Steroid Protocols
| Goal | Typical Steroid(s) Used | Reason |
|------|------------------------|--------|
| **Mass & Strength** | Testosterone, Trenbolone | Strong anabolic effect; high muscle protein synthesis |
| **Lean Muscle Definition** | Anavar (Oxandrolone), Winstrol (Stanozolol) | Mild anabolic activity with minimal water retention |
| **Performance Boost** | Nandrolone Decanoate, Boldenone | Enhances endurance and recovery |
| **Cutting / Fat Loss** | Testosterone + HGH + EPO | Supports lean muscle preservation while losing fat |
Steroids work by binding androgen receptors in cells, promoting transcription of genes that increase protein synthesis, reduce catabolism, and facilitate glycogen storage. They also influence the hypothalamic-pituitary-gonadal axis; at higher doses the body suppresses endogenous testosterone production (testosterone suppression). This can be mitigated with proper post-cycle therapy.
---
## 3. The "Best" Hormone for Physical Performance
> **Answer:**
> Testosterone, particularly in a transdermal or intramuscular form that delivers steady physiological levels, is considered the most effective hormone for boosting strength and endurance in healthy adults. It directly increases muscle protein synthesis, enhances red‑blood‑cell production (via EPO stimulation), improves neuromuscular function, and speeds recovery.
### Why Testosterone?
| Feature | Effect on Physical Performance |
|---------|--------------------------------|
| **Anabolic activity** | Stimulates satellite cell proliferation → larger muscle fibers. |
| **Nitrogen balance** | Maintains positive nitrogen status → promotes growth. |
| **Red‑cell production** | ↑ Hemoglobin → better oxygen delivery to muscles. |
| **Neuromuscular junctions** | Improves motor unit recruitment. |
| **Recovery** | Accelerates glycogen replenishment and reduces DOMS. |
### Types of Testosterone Preparations
| Preparation | Route | Pharmacokinetics | Practical Consideration |
|-------------|-------|------------------|-------------------------|
| Testosterone cypionate | Intramuscular | Long‑acting (2–4 weeks) | Requires fewer injections but risk of peaks/troughs. |
| Testosterone enanthate | IM | Similar to cypionate | Slightly shorter half‑life. |
| Testosterone undecanoate | Oral (capsules) | 1–2 days | Requires high-fat meals; variable absorption. |
| Transdermal gel | Topical | Daily dosing | Convenient, no injections; requires adherence. |
**Key points:**
- For athletes needing consistent testosterone levels with minimal monitoring, IM long‑acting esters or transdermal gels are common choices.
- Oral undecanoate is less favored due to variable absorption and the need for high-fat meals.
### 2.4 Clinical Indications for Testosterone Therapy
| Condition | Rationale for Testosterone Use |
|-----------|--------------------------------|
| **Hypogonadism** (primary/secondary) | Replace deficient hormone; improve libido, muscle mass, mood, bone density. |
| **Delayed puberty in males** | Initiate sexual development and secondary characteristics. |
| **Androgen Deficiency due to Chronic Illness** | Counteract catabolic state; improve quality of life. |
| **Gonadal Dysgenesis (e.g., Klinefelter syndrome)** | Support muscle mass, bone density, psychosocial development. |
| **Post‑menopausal androgen deficiency in women** | Treat fatigue, libido issues, and bone health (limited evidence). |
> **Side Note:** In men with prostate cancer or benign prostatic hyperplasia (BPH), systemic testosterone can exacerbate disease; careful monitoring is required.
---
## 3. Common Side Effects
| Category | Symptoms | Typical Onset | Management |
|----------|----------|---------------|------------|
| **Hormonal** | Acne, oily skin, increased body hair growth, voice deepening | 1–4 weeks after starting therapy | Topical retinoids, oral isotretinoin; discuss alternative formulations if severe |
| **Metabolic** | Weight gain, fluid retention (edema) | 2–6 weeks | Low-sodium diet, diuretics, monitor weight; consider adjusting dose |
| **Gastrointestinal** | Nausea, vomiting, bloating | Immediate to 1 week | Antiemetics, small frequent meals, avoid alcohol |
| **Renal** | Elevated serum creatinine, decreased urine output (rare) | Variable | Monitor renal function labs; adjust dosage accordingly |
| **Musculoskeletal** | Muscle cramps, myalgia | Weeks to months | Adequate hydration, electrolyte balance, consider supplements |
| **Hematologic** | Anemia, leukopenia (rare) | Variable | CBC monitoring; treat underlying causes |
| **Cardiovascular** | Hypertension, tachycardia (rare) | Weeks to months | Monitor BP, heart rate; adjust therapy as needed |
#### 2.3.2. Specific Considerations for Each Medication
- **Lisinopril**: Potential for cough, angioedema, hyperkalemia. Watch for renal function decline and electrolyte disturbances.
- **Hydrochlorothiazide**: Risk of hyponatremia, hypokalemia, dehydration, gout flares. Monitor electrolytes, renal function, and uric acid levels.
- **Metoprolol Succinate**: Bradycardia, hypotension, fatigue. Avoid in patients with significant bradyarrhythmias or heart block unless under cardiac monitoring.
---
## 3. Comprehensive Lifestyle Modification Plan
| Intervention | Target Goal | Key Actions |
|--------------|-------------|------------|
| **Weight Management** | Achieve and maintain BMI <25 kg/m² | - Calorie-controlled diet (<1500–1800 kcal/day)
- Portion control & mindful eating
- Track intake via food diary or app |
| **Physical Activity** | ≥150 min/week moderate aerobic + resistance training 2×/week | - Brisk walking, cycling, swimming (≥30 min ×5 days)
- Strength training: bodyweight exercises, resistance bands, light weights (≥8–12 reps ×3 sets)
- Flexibility & balance sessions |
| **Dietary Pattern** | Mediterranean-style diet | - Emphasize fruits, vegetables, whole grains, legumes, nuts
- Use olive oil as primary fat source
- Moderate fish and poultry; limit red meat
- Low-fat dairy or plant-based alternatives
- Limit sugary drinks & refined carbs |
| **Lifestyle Modifications** | Reduce sedentary time, manage stress | - Take short walks every hour during work
- Practice mindfulness/relaxation techniques (e.g., breathing exercises)
- Ensure 7–9 h of sleep per night |
---
## 3. How This Plan Helps
| **Goal** | **Why the plan works** |
|---|---|
| **Weight loss & improved body composition** | The moderate calorie deficit (~500 kcal/day) combined with resistance training promotes fat loss while preserving or increasing lean mass, leading to better metabolic health and insulin sensitivity. |
| **Lower fasting glucose & HbA1c** | Reducing caloric intake and improving diet quality decreases post‑prandial glucose spikes; regular exercise increases GLUT4 translocation in muscle cells, lowering basal blood sugar. |
| **Decreased risk of type 2 diabetes** | Evidence from large cohort studies (e.g., Diabetes Prevention Program) shows that a 5–10 % weight loss and at least 150 min/week of moderate‑intensity activity reduces progression to diabetes by ~58 %. |
| **Improved cardiovascular health** | Weight loss, dietary fats shift, and increased physical activity lower LDL cholesterol, blood pressure, and improve endothelial function. |
---
## Practical Guidance for a New Lifestyle
1. **Set SMART Goals**
- *Specific*: Lose 0.5–1 kg per week.
- *Measurable*: Track weight, waist circumference, food intake.
- *Achievable*: Start with 10‑minute walks and 2 servings of vegetables per meal.
- *Relevant*: Aligns with health priorities (cardiovascular risk reduction).
- *Time‑Bound*: Review every month.
2. **Meal Planning**
- **Breakfast**: Greek yogurt + berries + chia seeds.
- **Lunch**: Grilled chicken salad with mixed greens, olive oil vinaigrette.
- **Dinner**: Baked salmon + quinoa + steamed broccoli.
- Swap out high‑glycemic carbs (white rice, white bread) for whole grains.
3. **Physical Activity**
- Gradual increase: start with 10 min walking daily; add intervals of brisk walking or light jogging after a week.
- Include strength training twice per week using bodyweight exercises (squats, push‑ups).
4. **Monitoring & Feedback**
- Keep a food and activity log for 2 weeks to identify patterns.
- Use weight tracker weekly; adjust caloric intake by ~200 kcal if weight plateau occurs.
5. **Professional Support**
- Consider a brief consultation with a dietitian to personalize meal plans.
- If diabetes management is needed, coordinate with an endocrinologist for medication adjustments.
---
**Bottom‑Line Recommendation**
Adopt a modest calorie reduction (≈300 kcal/day) paired with increased physical activity and healthier food choices. Start gradually: incorporate 30‑minute brisk walks five times a week, replace sugary drinks with water or unsweetened tea, reduce portion sizes by ~10–15%, and choose whole‑grain or vegetable‑rich options. This balanced approach is sustainable, improves metabolic health, and can lead to gradual weight loss while supporting blood‑sugar control.
Let me know if you’d like a more detailed meal plan, exercise guide, or help with tracking progress! - https://remotejobscape.com/companies/sermorelin-vs-ipamorelin-comparing-two-leading-anti-aging-pepti
Artists to Follow
Weekly Top Tracks